Head and neck cancer screening
Surgeons and oncologists who work in Head and Neck Cancer Multidisciplinary Teams (MDTs) are qualified to screen patients for head and neck cancers. The process involves asking about possible symptoms, examining the mouth and the top of the throat with a good light source, and palpating the neck for lumps. Screening clinics which run outside traditional hospital environments are a great way to raise awareness of the signs and symptoms of these cancers, especially among people who may never have heard of the disease. Head and neck cancer screening also has one big advantage over many over screening clinics – we can examine the vast majority of patients without asking them to remove any items of clothing. In this blog I am sharing how we ran our screening clinic and what we learned in the hope that I can inspire other clinicians to do the same.
Clear objectives
The goal for our head and neck cancer screening clinic was to raise awareness. My practice team had been brainstorming ideas for activities for World Head and Neck Cancer Day (WHNCD) to help bring attention to these diseases. Not only do most people know very little about head and neck cancer but also the majority of those who have heard about it are under the false impression that the main contributing lifestyle factor is smoking. We were aware of other head and neck cancer screening clinics being run in hospitals which recruited volunteer patients who consisted mostly of hospital staff, visitors and some members of the public. We wanted to stage an event that was held off a hospital campus in order to engage with a broader cross section of the general public. The date for WHNCD is July 27 which meant that in 2019 WHNCD fell on a Saturday. Sports fields and shopping centres seemed like good options and we knew we wanted the screenings to be free. We had plenty of ideas but the difficulty was putting them into action.
Teamwork – look for partners and supporters
Fortunately for us we have been working for some time with Jennifer Holland and the team at Holland Healthcare. Jennifer is the inventor of Throat Scope, a tongue depressor with a light in it. Otolaryngology Head and Neck Surgeons (ENTs) routinely use specially designed light sources wen examining the mouth and throat. Not every doctor or clinician has access to this equipment. Throat Scope is a fantastic tool which enables GPs, dentists and other clinicians who regularly examine the mouth to complete a thorough oral examination without the need for a separate light source. Jennifer and her team had previously run an oral screening event in 2017 at the V8 Super Cars Newcastle. She offered to use her contacts to help us find a suitable venue to run our screening clinic on World Head and Neck Cancer Day. Jennifer did not disappoint and secured a spot for us at Bankwest Stadium among the pre-game activity during the National Rugby League premiership season when the Parramatta Eels played the New Zealand Warriors. We were stationed outside the main entrance. Thousands of people had to walk past our marquee to enter the stadium.

Bankwest Stadium Parramatta before the gates opened.
Before giving the project the green light we also approached Anthony Schembri AM, CEO of St Vincent’s Sydney and Dr Julia Maclean, president of the Australian New Zealand Head and Neck Cancer Society for their support. All clinicians participating in the event are members of both the St Vincent’s Head and Neck Cancer MDT and the ANZHNCS so it made sense to approach these organisations. St Vincent’s Sydney not only provided in principle support but also worked with me to create a video about neck lumps, one of the major symptoms of head and neck cancer, to run on St Vincent’s TV across their website and social media platforms on WHNCD.
You need a great team on your side
In order to run our free screening clinic we needed the following personnel;
- Qualified clinicians to complete the screening. This included myself, Otolaryngology Head and Neck Surgeon Dr Julia Crawford, and Dental Surgeon Dr Peter Foltyn, all members of the St Vincent’s Sydney Head and Neck Cancer Multidisciplinary Team (MDT).

St Vincents Sydney MDT clinicians Dr Julia Crawford, Dr Peter Foltyn, Dr Richard Gallagher.
- Clerical and admin team. Running a free screening clinic has the same risks and responsibilities for clinicians as seeing patients in a regular practice setting. Our clerical and admin team greeted patients, made sure they completed the appropriate paperwork, kept supplies up to clinicians, and ensured those patients with a suspected underlying diagnosis were appropriately referred for follow up;
- Thank goodness for Jennifer and her team at Holland Healthcare. They provided the marquee, Throat Scopes and disposable blades, furniture, screen dividers, gloves, gauze, hand sanitizer, waste containers and every other piece of equipment we needed to perform examinations.
- Patient recruiters. We were lucky to have a great team of volunteer patient recruiters who not only approached members of the public for screening but also shared literature with them about the free clinic and head and neck cancers. Their friendly, pressure-free approach ensured that a number of members of the public who originally said ‘no thank you’ returned to participate once they had read more about the screening clinic on the information postcard.
Logistics and patient literature
One major advantage of screening for head and neck cancer over screening for cancers on other sites of the body is that very few items of clothing need to be removed. That said, I admired a lot of Parramatta Eels beanies and scarves. But we still wanted to provide privacy to patients and created individual screening booths. In addition to a weather proof marquee, examination equipment and furniture we also needed banners, signage and patient literature. The banners and signs communicated what we were doing and the literature ensured people understood the screening process, the signs and symptoms of head and neck cancer, and where to find more information. Jennifer had the great idea of putting this information in the form of a postcard which included a link to the excellent online Head and Neck Cancer resources at the NSW Cancer Council
.

Each clinician worked in a screened consultation area within the marquee.
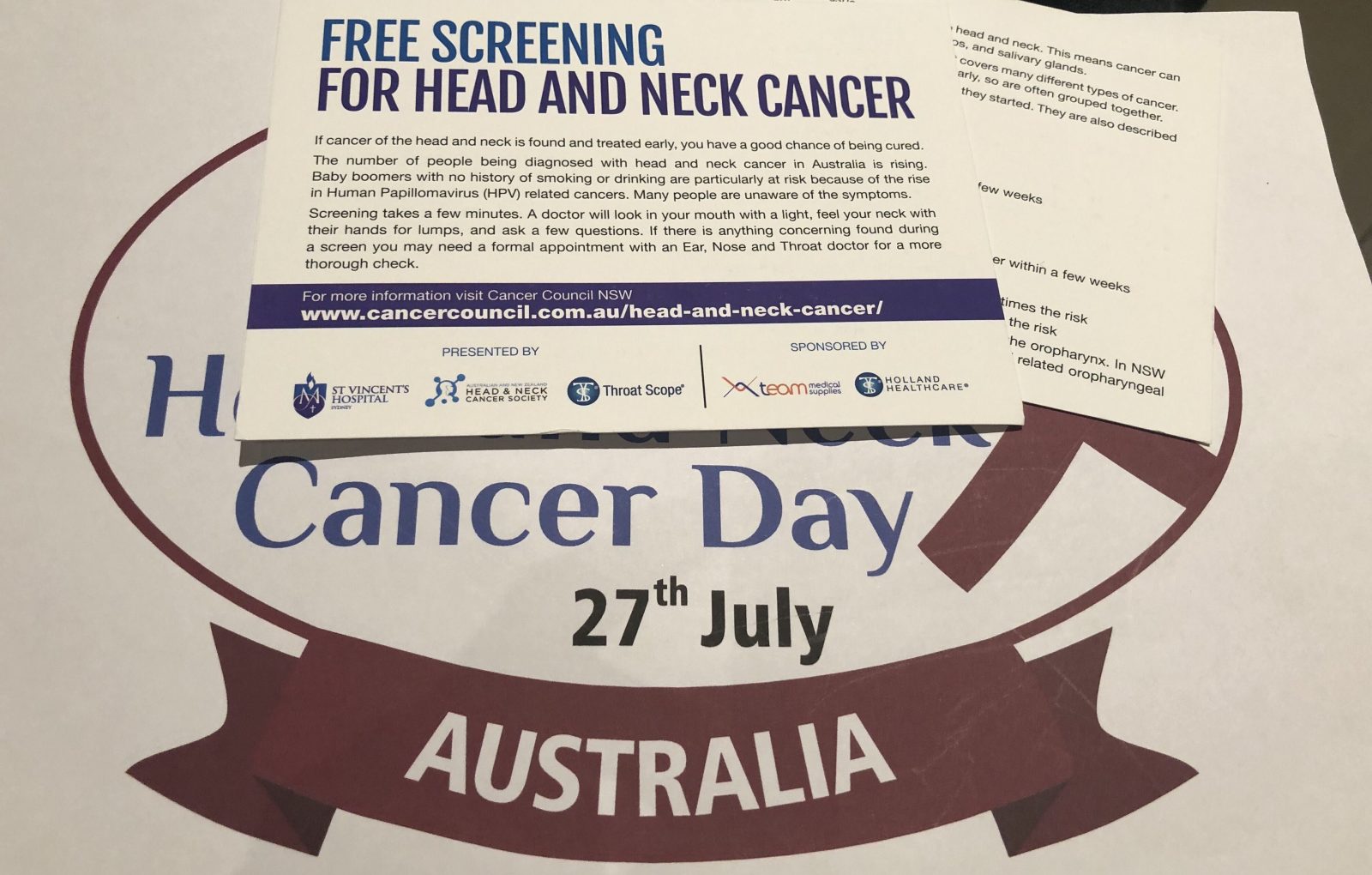
Literature needs to be easy to read and provide links to authority sources.
Medico-legal risks and public liability
Running a pop up screening clinic is not risk free for patients, organisers or clinicians. We took advice from Avant Risk Management to ensure we understood what we were getting ourselves into. Patients who see clinicians at a free screening clinic like ours have the right to expect the same standard of care as they would if they were seeing the clinician at a pre-arranged appointment in a practice or hospital setting. We had to collect patient data, display a privacy policy explaining what would happen to that data, record the findings for each patient, and provide a letter for patients with an underlying suspected diagnosis to take to their regular GP for follow up. We only screened people over eighteen years of age. There was no power supply to our marquee so all of this had to be done by hand with pre-printed paper templates. Over the next few days my staff will enter all patient details into our patient database, scan and link records of each consultation to create a medical record, and follow up patients with a suspected underlying diagnosis to ensure they get the care they need. Medical records from the event will be retained in digital format in our secure system for the next seven years in accordance with medical record storage regulations and the paper versions will be appropriately destroyed in order to protect patient privacy. The staff at Bankwest Stadium were a pleasure to liaise with and made sure we met our responsibilities of providing a certificate of currency for public liability and that our marquee was weighted securely in case of severe wind gusts. We were very lucky with the weather, it was a spectacular winter’s day. We also had to remove our own rubbish and follow explicit set up instructions regarding access.
How did it go? What did we find?
We screened just over one hundred patients in two and a half hours, including the Parramatta Eels cheer squad, Life Education Ambassador Healthy Harold, being a giraffe his neck examination took a little longer than average, and three fine members of the NSW Police Force. There was no shortage of patients. The Parramatta Eels supporters were out in force with over 17,000 people attending the game. We identified four patients with suspected underlying diagnoses, 4% of our patient cohort. The findings included enlarged lymph nodes in the neck and lip lesions. These patients were either unaware of their symptoms or unaware their symptoms required further investigation. Not surprisingly the group of Eels supporters smoking around the corner from us were reluctant to participate in the screening clinic. To their credit, they did take our literature and thanked us for the invitation.

Dr Julia completing a slightly tricky examination.

Police officers participating in screening after checking the 17,000 strong crowd was safely in the stadium.
Was the day a success?
Yes, this event was definitely a success, we achieved our goal of raising awareness of head and neck cancers, not just among the patients we examined but also among people with whom we had conversations and to whom we distributed printed information. I will also say that it was not just the patients who benefitted. My team and I had an exhausting but uplifting day getting out of our regular environment and talking to a huge range of people about these rare cancers. It was rewarding to reassure those patients who were scared of what we might find when they volunteered to be examined, and it was delightful to screen patients who were happy and relaxed, an unusual experience for someone like me who spends most days diagnosing cancer. Our findings of four patients requiring follow up confirms that we interacted with a general cross section of the population.
Would we do it again?
Definitely. We look forward to doing other free Head and Neck Cancer screening events in the future. In the public conversation about cancer neither head and neck cancer nor head and neck cancer patients receive the attention or funding they deserve. Taking direct action to screen one hundred people may sound like a drop in the ocean but the success of the event only strengthened me and my teams’ resolve to keep working to raise awareness. If clinicians like me don’t do it who will.

The entire head and neck cancer clinic screening team – three support members to every one clinician.




